Exploring the Procedure: A Step by Step Guide to TAVI
02/15/2024
Purpose Of TAVI
The aortic valve typically opens as blood is pushed from your heart to the rest of your body. Aortic stenosis is a condition in which the aortic valve does not open and close normally. This abnormality puts extra strain on your heart and can cause dyspnea, swelling ankles, chest pain, disorientation, and, in extreme cases, blackouts.
The primary treatment for aortic valve issues is open heart valve surgery. However, open-heart surgery may be considered too dangerous for patients who are too ill or have several other medical issues.
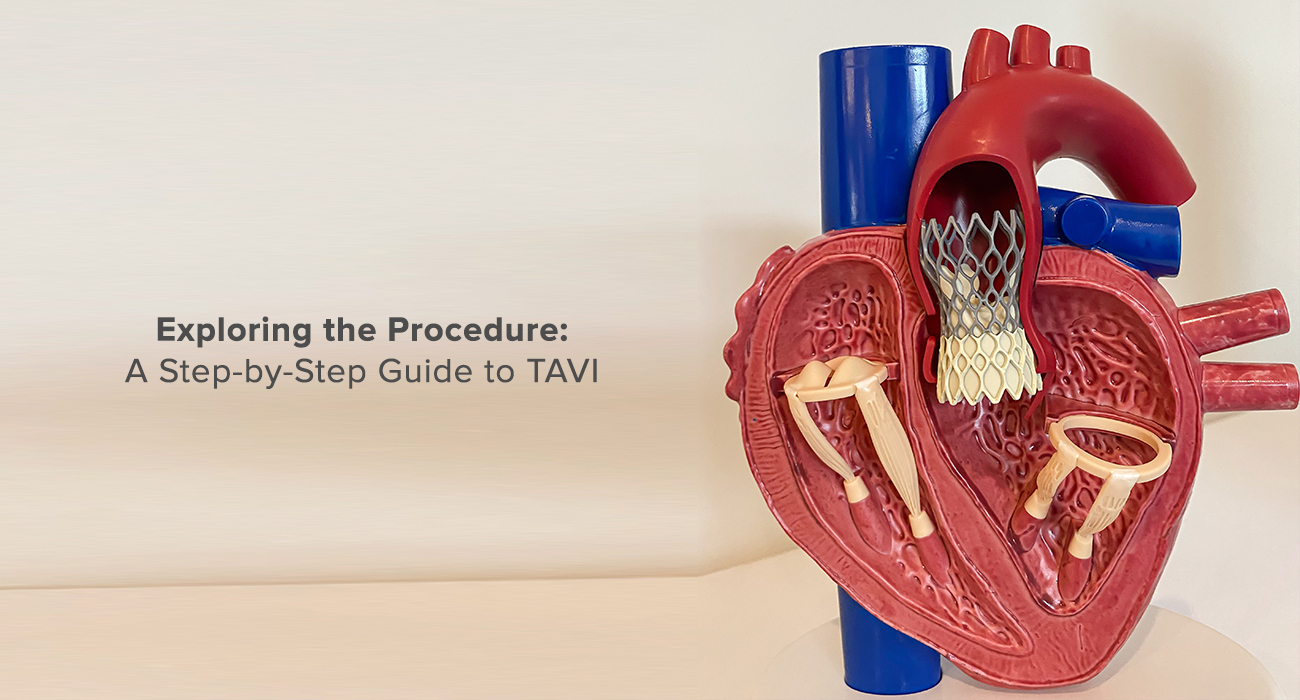
Transcatheter aortic valve implantation (TAVI) is a surgery that involves implanting an aortic valve using a long, narrow tube known as a catheter.
Typically, the catheter is put into a large blood vessel in the groin or through a tiny cut in the chest. Transcatheter aortic valves are designed specifically for this surgery. To insert a valve into the heart, it is pressed around or inside a catheter. The catheter is then inserted and guided to the aortic valve opening in your heart, where it is placed over your current valve. After the new valve is installed, the catheter is withdrawn. The replacement valve starts working immediately.
Steps For TAVI
Before TAVI
- You will be admitted to the cardiac department one day before the procedure.
- You will be asked to sign a consent form.
- On the day of your procedure, you will be taken to the cardiac cath lab.
- Preoperative:
During your preoperative visit, your assigned healthcare professional will provide you with a list of instructions that are specific to you.
- The day of the procedure
After checking in with the admitting office, you will be escorted to the preoperative area to begin preparations for the surgery.
An IV and an arterial line will be put in the preoperative area to deliver medications and fluids while also monitoring blood pressure.
During TAVI
- Preparing the Site: First, all puncture sites are injected with a local anesthetic. The right jugular vein is readily available with ultrasound guidance and a micropuncture needle, followed by the placement of a tearaway sheath over the wire. A wire is inserted into the apex of the right ventricle. Ultrasound guidance and a micropuncture needle are then utilized to locate the common femoral artery on the other side of the TAVI access. Next, an incision is made above the femoral artery on the TAVI side so that the vascular closure device can easily reach the artery. An arteriogram is then performed to confirm that the access is as required and not any other position.
- Checklist: Two checklists are used throughout the procedure to ensure all steps are followed. One is used after the placement of the access sheath and the other before implanting the valve.
- Balloon test (optional): A pre-implant balloon valvuloplasty is then carried out, typically with a noncompliant balloon sized to the patient’s anatomy. This is not always necessary but is preferred when the valve is heavily calcified and for all patients with bicuspid aortic valves. The transcatheter valve is then checked under fluoroscopy to make sure it has been loaded well before it is inserted.
- Introducing the new valve: The surgeons carefully advance the transcatheter heart valve (THV) across the native valve. With the marker band centered, the deployment of the valve itself has begun. As the valve exits the sheath, implant depth is assessed, as the valve is not yet fully deployed. The depth in the cusp overlap view is verified. The surgeons reassess the depth and then wait between two and four minutes for the valve to expand. While doing so, an echo is recorded to confirm the depth on both the mitral and septal sides.
- Placing the new valve: Once the surgeons are satisfied with the position, they release the valve. The nose cone is then carefully centralized to avoid dislodging the valve, and the delivery system is taken out. A root angiography and hemodynamics are done to confirm there is no residual left. This is also confirmed by echoing with a color Doppler. The TAVI sheath is withdrawn over the wire while the dilator remains in place.
- Checking and finishing: A tourniquet can be utilized to provide temporary hemostasis when employing the preclose technique. Reassessment of the bleeding site is done at the access site after approximately two minutes of protamine (an anticoagulant reversal agent) administration. A complete angiography is then done on the access vessel to establish normal flow and the absence of any new disease. If the patient has a normal rhythm and a narrow complex with no new conduction problems, the surgeons will remove the temporary transvenous pacemaker. Otherwise, the TVP is left in place overnight with a backup rate of 40 bpm and is reassessed the following morning. The patient is subsequently brought to the post-anesthesia area.
- After TAVI: Following the procedure, you will be monitored in the Surgical Intensive Care Unit for at least 24 hours. You will be awakened and transferred to your recovery room to recuperate from the anesthetic. Usually, you'll stay in bed for the first four hours. If a temporary pacemaker is left in place, you will be on bed rest until it can be safely removed.Once stable, you can be transferred to a regular ward, where you will recuperate and prepare for discharge during the next five to ten days.
Conclusion:
Transcatheter Aortic Valve Implantation (TAVI) is a minimally invasive treatment for constricted aortic valves, eliminating the need for open-heart surgery. This minimally invasive treatment uses tiny catheters and a deflated replacement valve to reach and replace the defective valve within your heart, providing multiple advantages. Compared to open-heart surgery, TAVI allows patients to return home within a few days. The tiny incision and catheter-based method reduce tissue damage and pain.